Why Your Doctor Doesn’t Rush to Prescribe Antibiotics for Colds and Coughs
If you’ve ever gone to the doctor feeling miserable- coughing, congested, exhausted- and left without an antibiotic, you’re not alone in feeling frustrated.
Many patients worry that “nothing was done,” or that their illness will linger without medication. In reality, choosing not to prescribe antibiotics is often a deliberate, evidence-based decision made in your best interest.
Let’s talk about why.
Most Coughs and Colds Are Viral, Not Bacterial
The majority of upper respiratory infections- colds, bronchitis, sinus congestion, sore throats- are caused by viruses, not bacteria.
Antibiotics only work against bacteria. When used for viral illnesses, they:
Don’t shorten the illness
Don’t reduce complications
Can cause side effects like diarrhea, yeast overgrowth, and allergic reactions
Disrupt the gut microbiome, which plays a key role in immune function
In other words, antibiotics aren’t “stronger medicine” for these situations—they’re the wrong tool.
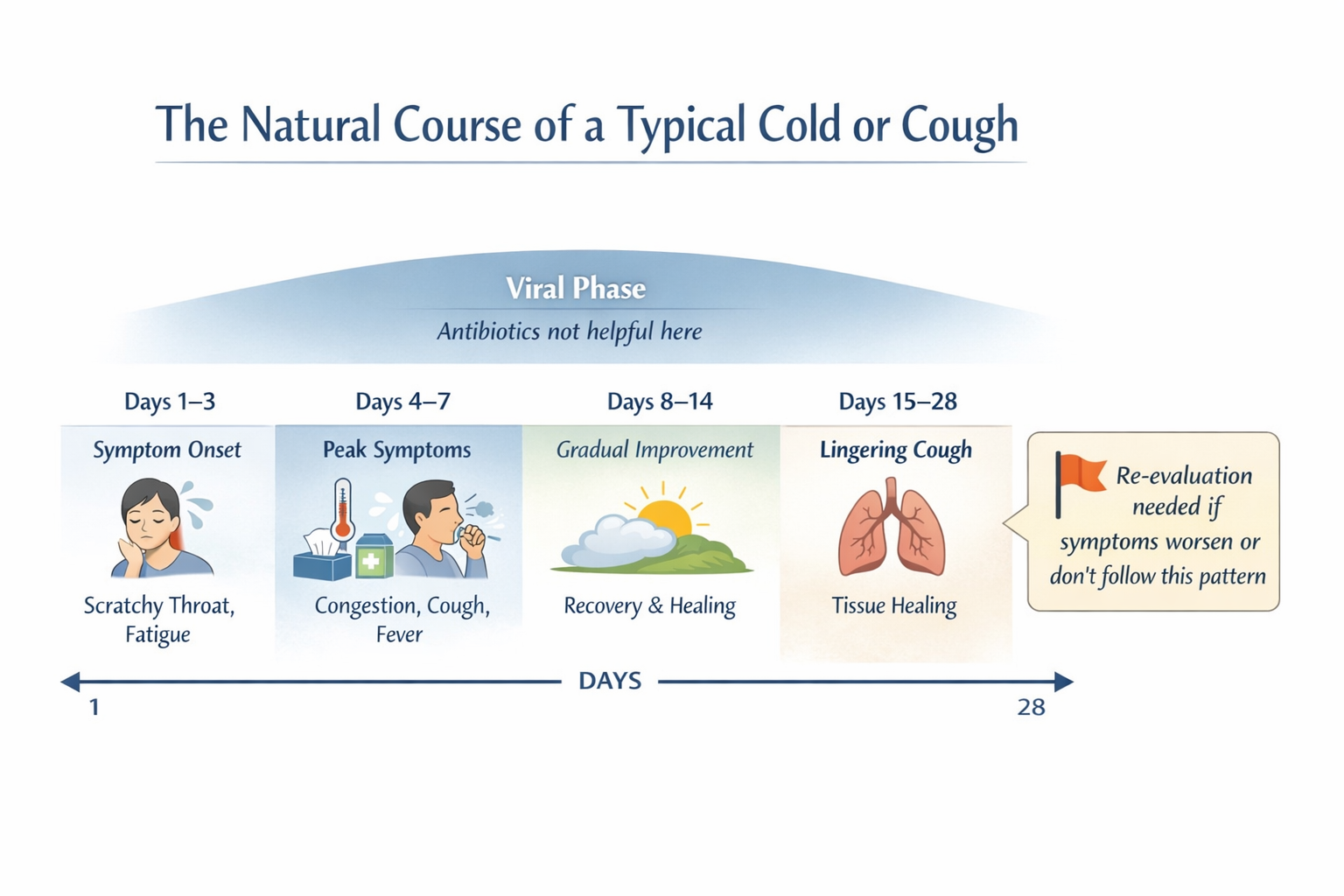
Illness Has a Natural Progression
Coughs and colds tend to follow a predictable pattern:
Symptoms build over several days
Peak when your immune system is actively fighting
Gradually improve as inflammation settles and tissues heal
A lingering cough can last 2–4 weeks, even when recovery is progressing normally. This doesn’t mean the body is failing—it often means it’s finishing the repair process.
Prescribing antibiotics too early can interfere with this natural immune response rather than support it.
Why “Just in Case” Antibiotics Can Backfire
Using antibiotics when they aren’t clearly indicated increases the risk of:
Antibiotic resistance (making future infections harder to treat)
Recurrent infections
Gut and vaginal yeast overgrowth
Long-term microbiome disruption, which can affect digestion, immunity, and inflammation
From a whole-body perspective, restraint is often the safer choice.
What Does Help Instead
When antibiotics aren’t appropriate, care still matters. At KlarCare, we focus on:
Improving the anatomy so lymph can appropriately drain and the lungs can properly pump healing fluids to and junk away from infected areas;
Improving nutrition (big nutrients are vitamin C, zinc, and D!) to give you immune system the upper hand,
Monitoring symptoms closely over time
Supporting the immune system and recovery
Addressing inflammation, hydration, sleep, and nutrition
Watching for specific signs that would suggest a bacterial infection and a change in plan
This approach reduces unnecessary medications while ensuring you don’t miss something important.
When Antibiotics Are the Right Choice
There are absolutely times when antibiotics are appropriate—and when they are, we use them thoughtfully and decisively.
Signs that may prompt antibiotic treatment include:
Symptoms that worsen after initial improvement
Persistent high fevers
Focal findings on exam suggesting bacterial infection
Clear clinical patterns that don’t fit a viral course
The key is timing and context, not reflexive prescribing.
The Bottom Line
Not prescribing an antibiotic isn’t dismissal, it’s discernment.
Good medicine isn’t about doing something at every visit. It’s about doing the right thing, at the right time, for the right reason, while protecting your long-term health.
If you’re ever unsure why a particular approach is being recommended, ask. A good doctor should always be willing to explain the “why.”